 Steven Webb, President, Workers’ Compensation, Express Scripts
Steven Webb, President, Workers’ Compensation, Express Scripts
…on the need for a team approach to opioid management
There’s no silver bullet to manage the safety and cost concerns associated with opioid use. At Express Scripts, we help payers fire on all cylinders.
For example, our Morphine Equivalent Dose Management Program is a real-time safety check to prevent abuse or misuse of opioids before medication is dispensed.
We also have a program in place to communicate directly with the injured worker upon their first opioid fill.
And we collaborate with claims staff and prescribing physicians through various tools and communications to ensure comprehensive visibility into the injured workers’ prescription histories.
When payers proactively arm themselves with tools that hit every touch point, they help ensure safe and cost-effective treatment for their injured workers.
Upcoming Webinar: Insights from the 2014 Workers’ Compensation Drug Trend Report from Express Scripts Experts: May 21, 2015 at 11:00 CDT.
___________________________________________________________________________________________
Workers’ Compensation Rx Spend Increased 1.9{ac84179ccc1556745dd38e14876b163ce042b824eb5390d08aeb8a9ee8786546} in 2014
While rising costs per prescription is still a concern, Express Scripts’ effective utilization management programs helped to stabilize the increase in drug trend.
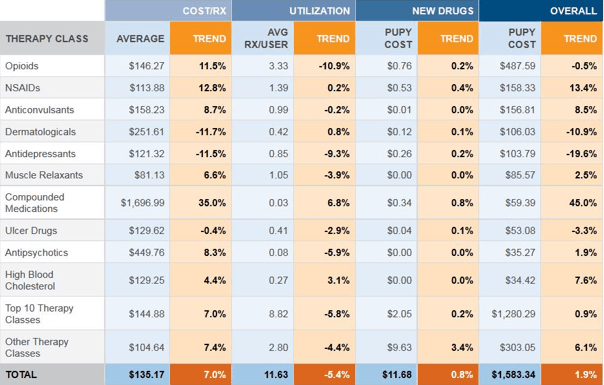
Overall drug trend for workers’ compensation increased 1.9{ac84179ccc1556745dd38e14876b163ce042b824eb5390d08aeb8a9ee8786546}, according to the 9th Annual Express Scripts Workers’ Compensation Drug Trend Report.
A 5.4{ac84179ccc1556745dd38e14876b163ce042b824eb5390d08aeb8a9ee8786546} decrease in utilization helped offset a 7{ac84179ccc1556745dd38e14876b163ce042b824eb5390d08aeb8a9ee8786546} increase in the cost per prescription.
TOP 10 WORKERS’ COMPENSATION THERAPY CLASSES
Opioid Management Mitigates Spend Increases
The modest increase in overall pharmacy spend demonstrates the effectiveness of Express Scripts utilization management programs. In fact, opioid utilization among injured workers decreased nearly 11{ac84179ccc1556745dd38e14876b163ce042b824eb5390d08aeb8a9ee8786546} in 2014.
As drug prices continue to increase, payers – now more than ever – are looking to contain costs by implementing effective programs that ensure safe and appropriate use of opioids.
Our data-driven solutions help payers meet this goal. For example, the Express Scripts Morphine Equivalent Dose (MED) Management program allows our clients to set maximum threshold levels for the amount of opioid medications an injured worker can fill. Amounts exceeding MED program levels undergo a review process by the client before the medication is dispensed.
According to the Washington State Agency Medical Directors’ Group (AMDG), patients receiving an MED of 100mg or more per day had a nine-fold increase in overdose risk. Our research found that more than one fifth of patients with work-related injuries longer than 15 years exceeded the MED of 120mg per day on more than half of the days for which opioid medications were being filled.
INJURED WORKERS PRESCRIBED OPIOID THERAPY WITH MED ? 120 MG

Although older injuries may require higher doses of opioids because the patient has become tolerant to previous doses, patients receiving an MED of 100mg or more raises serious concerns about the potential of addiction and abuse. Better management of opioid use among injured workers helps to reduce abuse, limit addiction and control costs.
Combatting Rising Compounded Medication Costs
For the second year in a row, compounded medications were one of the top 10 costliest therapy classes for workers’ compensation payers.
Unsustainable pricing greatly impacted the overall trend, and the average cost of compounds per prescription in 2014 was $1,696.99.
Our research found that pharmacies who compound more than two-thirds of their total prescriptions increased their prices 51.5{ac84179ccc1556745dd38e14876b163ce042b824eb5390d08aeb8a9ee8786546} in 2014. Low-compounding pharmacies – or those than compounded less than 67{ac84179ccc1556745dd38e14876b163ce042b824eb5390d08aeb8a9ee8786546} of their total prescriptions – averaged only a 9.7{ac84179ccc1556745dd38e14876b163ce042b824eb5390d08aeb8a9ee8786546} price increase.
MEDIAN COSTS OF COMPOUNDED PRESCRIPTIONS FILLED
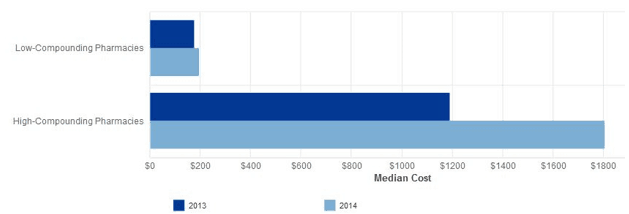
Our research also found that 10{ac84179ccc1556745dd38e14876b163ce042b824eb5390d08aeb8a9ee8786546} of compound utilizers did not receive a traditional prescription before receiving their compounded medication – that is, they used a compounded medication as the first prescription for their injury.
This raises the question of why first-line therapies were not tried first. While accommodating needs for a patient who cannot ingest or is allergic to available alternatives is appropriate, there is no clinical evidence that compounded medications are more effective than FDA-approved, commercially available drugs.
Compound Management Solution
At the point of sale, Express Scripts workers’ compensation clients have the option of reviewing all compounds for authorization. Retrospectively, we communicate to physicians and injured workers encouraging the use of commercially available, cost-effective alternatives where appropriate.
When payers implement the physician communications program, 46.6{ac84179ccc1556745dd38e14876b163ce042b824eb5390d08aeb8a9ee8786546} of their injured workers discontinued filling unnecessary compounded medications.
Reining in the Cost of Physician Dispensing
Medication dispensed through a physician’s office not only has a higher cost than if dispensed through a retail pharmacy, it also lacks a comprehensive view of a patient’s prescription history and profile. Without the checks and balances between prescriptions and pharmacists, injured workers are at risk for medication errors, drug interactions and duplicate dosing.
Our research found that the average cost of a physician-dispensed medication in 2014 was $173.75, compared to $111.68 for a pharmacy-dispensed medication.
This means that clients paid an average premium of about $62 per prescription for physician-dispensed medications.
Express Scripts’ Physician Dispensed Medication Solution helps to tackle the cost and utilization of physician dispensing.
The Reality Behind Generic Drug Inflation
Although price inflation for a few generic drugs has captured media attention recently, it is not a new phenomenon. There are two primary drivers of the inflation in generic drug pricing: manufacturer consolidation and temporary shortages of active ingredients.
While it’s true that the price for some generics have increased, on the whole, generic medications continue to deliver significant cost savings by providing cost-effective alternatives to brand name medications. Consider that since 2008, the average price of brand drugs has almost doubled, while the average price of generic drugs has been cut roughly in half.
THE EXPRESS SCRIPTS PRESCRIPTION PRICE INDEX
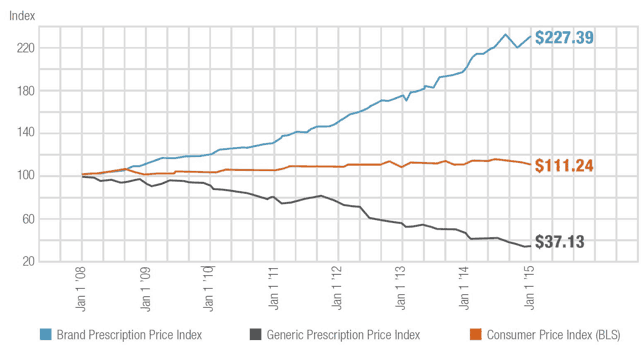
Express Scripts helps lower drug costs by driving competition in the market and by leveraging our scale to drive the best prices for payers. In general, encouraging use of generics over more expensive brand alternatives, when clinically appropriate, is still an effective way for payers to keep costs down.
Express Scripts research found that for every 1{ac84179ccc1556745dd38e14876b163ce042b824eb5390d08aeb8a9ee8786546} increase in the generic fill rate, a payer can expect to reduce prescription drug costs by as much as 2{ac84179ccc1556745dd38e14876b163ce042b824eb5390d08aeb8a9ee8786546}.
Understanding Specialty Trend
Specialty medications treat relatively small groups of patients with complex, chronic conditions. These drugs are typically are very expensive and most have special-handling requirements. In addition, patients taking specialty medications may need ongoing clinical monitoring and more-intensive assistance and guidance from pharmacists or other caregivers.
Many occupations have specific risks such as HIV, hepatitis C, or other blood-borne pathogens resulting from needle sticks or other exposures (healthcare providers and first responders), black lung disease (coal miners), and Lyme disease (outdoor workers/landscapers or park employees). Additionally, some consequential conditions, including post-operative blood clots, osteoarthritis knee pain and even organ failure, are treated with specialty medications.
Although specialty medications represent less than 1{ac84179ccc1556745dd38e14876b163ce042b824eb5390d08aeb8a9ee8786546} of all medications used by injured workers, they have the potential to increase drug spend significantly because their costs are rising rapidly. Between 2013 and 2014, spend on specialty medications increased 30.4{ac84179ccc1556745dd38e14876b163ce042b824eb5390d08aeb8a9ee8786546}. New specialty medications offer clinical options for the treatment of occupational injuries and the hope of improved medical outcomes, but the cost pressures they present prove challenging to payers in the management of these medications.
For example, drugs to treat hepatitis C, Sovaldi® (sofosbuvir) and Olysio® (simeprevir), had the highest cost per prescription, with average cost upwards of $20,000 per 28-day prescription. Sovaldi alone accounted for more than 57{ac84179ccc1556745dd38e14876b163ce042b824eb5390d08aeb8a9ee8786546} of the new-drug contribution to 2014 PUPY specialty spend.
Author:
Rochelle Henderson, PhD, is Senior Director of Research for Express Scripts, Inc. In this capacity, she supervises a team of Ph. D. heath policy researchers and works with schools of pharmacy and medical schools in the greater St. Louis area. She serves on a number of health related research teams with institutions across the St. Louis region: Washington University School of Medicine with Barnes Hospital, the Veteran’s Administration Regional Hospital, and with the School of Nursing from Southern Illinois University at Edwardsville (SIUE). Dr. Henderson holds an adjunct faculty position at SIUE, teaching courses in epidemiology and quantitative analysis. She has 20 years of experience in pharmacoepidemiologic and pharmacoeconomic research. Dr. Henderson also has extensive publishing credits, including numerous peer-reviewed articles in American Journal of Managed Care, Journal of Managed Care Pharmacy, Annals of Pharmocotherapy, Clinical Therapeutics, and other prestigious journals. Dr. Henderson received her Doctorate from the University of Missouri – St. Louis.
The post Overall Drug Trend For Workers’ Compensation Increased 1.9{ac84179ccc1556745dd38e14876b163ce042b824eb5390d08aeb8a9ee8786546} appeared first on Work Comp Roundup.
SOURCE: Work Comp Roundup – Read entire story here.

